THRIVE (Transforming Health through Real-world Insights, Values and Evidence) is Dr. McCoy’s interdisciplinary research program focused on improving care delivery and health outcomes for people living with diabetes and its comorbidities, housed within the UM-IHC Center for Population Health.
Our Faculty
Rozalina G. McCoy, MD MS (Director, UM-IHC Center for Population Health)
Dr. McCoy is an endocrinologist, internist, and health services researcher with a passion for improving the quality, accessibility, and sustainability of medical care for people living with diabetes and other chronic conditions, particularly those with clinical complexity and structural barriers to evidence-based care and health. Broadly, her work relies on using real-world data and a wide range of observational, quasi-experimental, and mixed methods designs to 1) characterize, identify, and predict high-risk subgroups; 2) identify treatment strategies that yield optimal health outcomes with least burden of treatment, harm, and cost; 3) operationalize the sustainable delivery of person-centered care in clinical and community settings; and 4) facilitate patient and other stakeholder engagement in research.
Her recent work has focused on 1) epidemiology and prediction of acute and chronic diabetes complications; 2) impacts of social and structural determinants of health (e.g. area-level deprivation, rurality, income, health benefit design) on diabetes care and outcomes; 3) emulating comparative effectiveness trials of diabetes, obesity, and osteoporosis therapies; 4) primary care, organizational, and payment models associated with optimal diabetes care and outcomes; and 5) design, implementation, and evaluation of novel care models for high-risk patients, such as mobile integrated health, comprehensive and team-based primary care, and transitional care programs.
Dr. McCoy is also an internationally recognized leader in diabetes management and has chaired the American Diabetes Association Professional Practice Committee since 2024. Her research has been funded by the National Institutes of Health (NIH), the Patient-Centered Outcomes Research Institute (PCORI), the American Diabetes Association, the U.S. Food and Drug Administration (FDA), and the U.S. Department of Defense. She has published >250 peer-reviewed publications and mentored >35 faculty and trainees across different disciplines and specialties.
Some of her work includes:
- McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care. 2012; 35(9):1897-1901. [PMC3425008]
- McCoy RG, Lipska KJ, Yao X, Ross JS, Montori VM, Shah ND. Intensive treatment and severe hypoglycemia among adults with type 2 diabetes. JAMA Intern Med. 2016; 176(7):969-978. [PMC5380118]
- McCoy RG, Lipska KJ, Van Houten HK, Shah ND. Association of Cumulative Multimorbidity, Glycemic Control, and Medication Use With Hypoglycemia-Related Emergency Department Visits and Hospitalizations Among Adults With Diabetes. JAMA Netw Open. 2020;3(1):e1919099. [PMC6991264]
- McCoy RG, Galindo RJ, Swarna KS, Van Houten HK, O’Connor PJ, Umpierrez GE, Shah ND. Sociodemographic, Clinical, and Treatment-Related Factors Associated With Hyperglycemic Crises Among Adults With Type 1 or Type 2 Diabetes in the US From 2014 to 2020. JAMA Netw Open. 2021;4(9):e2123471. [PMC8411297]
- Umpierrez GE, Davis GM, ElSayed NA, Fadini GP, Galindo RJ, Hirsch IB, Klonoff DC, McCoy RG, Misra S, Gabbay RA, Bannuru RR, Dhatariya KK. Hyperglycemic Crises in Adults With Diabetes: A Consensus Report. Diabetes Care. 2024;47(8):1257-1275. [PMC11272983]
- Rodriguez-Gutierrez R, Gonzalez-Gonzalez JG, Zuñiga-Hernandez JA, McCoy RG. Benefits and harms of intensive glycemic control in patients with type 2 diabetes. BMJ. 2019;367:l5887.
- Jiang DH, O’Connor PJ, Huguet N, Golden SH, McCoy RG. Modernizing Diabetes Care Quality Measures. Health Aff. 2022;41(7):955-962. [PMC9288231]
- Herges JR, Matulis JC 3rd, Kessler ME, Ruehmann LL, Mara KC, McCoy RG. Evaluation of an Enhanced Primary Care Team Model to Improve Diabetes Care. Ann Fam Med. 2022;20(6):505-511. [PMC9705037]
- Paulson MR, Shulman EP, Dunn AN, Fazio JR, Habermann EB, Matcha GV, McCoy RG, Pagan RJ, Maniaci MJ. Implementation of a virtual and in-person hybrid hospital-at-home model in two geographically separate regions utilizing a single command center: a descriptive cohort study. BMC Health Serv Res. 2023;23(1):139. [PMC9911182]
- Matulis JC 3rd, Swanson K, McCoy R. The association between primary care appointment lengths and opioid prescribing for common pain conditions. BMC Health Serv Res. 2024;24(1):776 [PMC11220962]
- Deng Y, Polley EC, Wallach JD, Dhruva SS, Herrin J, Quinto K, Gandotra C, Crown W, Noseworthy P, Yao X, Lyon TD, Shah ND, Ross JS, McCoy RG. Emulating the GRADE trial using real world data: retrospective comparative effectiveness study. BMJ. 2022; 379:e070717. [PMC9527635]
- McCoy RG, Herrin J, Swarna KS, Deng Y, Kent D, Ross JS, Umpierrez G, Galindo RJ, Crown W, Borah B, Montori, VM, Brito Campana JP, Neumiller JJ, Mickelson M, Polley EC. Effectiveness of Glucose-Lowering Medications on Cardiovascular Outcomes in Patients with Type 2 Diabetes at Moderate Cardiovascular Risk. Nature Cardiovascular Research. 2024;3(4):431-440
- Barkmeier AJ, Herrin J, Swarna KS, Deng Y, Polley EC, Umpierrez GE, Gallindo RJ, Ross JS, Mickelson MM, McCoy RG. Comparative Effectiveness of GLP-1 Receptor Agonists, SGLT2 Inhibitors, DPP-4 Inhibitors, and Sulfonylureas for Sight-Threatening Diabetic Retinopathy. Ophthalmol Retina. 2024:S2468-6530(24)00229-X
- Neumiller JJ, Herrin J, Swarna KS, Polley EC, Galindo RJ, Umpierrez GE, Deng Y, Ross JS, Mickelson MM, McCoy RG. Kidney Outcomes with Glucagon-Like Peptide-1 Receptor Agonists, Sodium-Glucose Cotransporter 2 Inhibitors, Dipeptidyl Peptidase-4 Inhibitors, and Sulfonylureas in Type 2 Diabetes and Moderate Cardiovascular Risk. Clin J Am Soc Nephrol. 2024 Oct 8.
- Brito JP, Herrin J, Swarna KS, Singh Ospina NM, Montori VM, Toro-Tobon D, Umpierrez GE, Galindo RJ, Deng Y, Mickelson MM, Shao H, Polley EC, McCoy RG. GLP-1RA Use and Thyroid Cancer Risk. JAMA Otolaryngol Head Neck Surg. 2025 Jan 23;
- McCoy RG, Van Houten HK, Ross JS, Montori VM, Shah ND. HbA1c overtesting and overtreatment among US adults with controlled type 2 diabetes, 2001-13: observational population based study. BMJ. 2015; 351:h6138. [PMC4673101].
- Allen AM, Van Houten HK, Sangaralingham LR, Talwalkar JA, McCoy RG. Healthcare Cost and Utilization in Nonalcoholic Fatty Liver Disease: Real-World Data From a Large U.S. Claims Database. Hepatology. 2018;68(6):2230-2238. [PMC6240503]
- Maraka S, Mwangi R, Yao X, Sangaralingham LR, Singh Ospina NM, O’Keeffe DT, Rodriguez-Gutierrez R, Stan MN, Brito JP, Montori VM, McCoy RG. Variation in treatment practices for subclinical hypothyroidism in pregnancy: US national assessment. J Clin Endocrinol Metab. 2019;104(9):3893-3901. [PMC6667278]
- Kurani S, Jeffery MM, Thorsteinsdottir B, Hickson LJ, Barreto EF, Haag J, Giblon R, Shah ND, McCoy RG. Use of Potentially Nephrotoxic Medications by U.S. Adults with Chronic Kidney Disease: NHANES, 2011-2016. J Gen Intern Med. 2020;35(4):1092-1101. [PMC7174522]
- McCoy RG, Van Houten HK, Karaca-Mandic P, Ross JS, Montori VM, Shah ND. Second-Line Therapy for Type 2 Diabetes Management: The Treatment/Benefit Paradox of Cardiovascular and Kidney Comorbidities. Diabetes Care. 2021;44(10):2302-11. [PMC8929191]
- Herges JR, Galindo RJ, Neumiller JJ, Heien HC, Umpierrez GE, McCoy RG. Glucagon Prescribing and Costs Among U.S. Adults With Diabetes, 2011-2021. Diabetes Care. 2023 ;46(3):620-627. [PMC10020025]
- Galindo RJ, Inselman SA, Umpierrez GE, Moazzami B, Munoz Mendoza J, Ali MK, Tuttle KR, McCoy RG. National Trends in Glucagon Prescriptions Among U.S. Adults With Diabetes and End-Stage Kidney Disease Treated by Dialysis: 2013-2017. Diabetes Care. 2023;46(7):e130-e132. [PMC10300513]
- Herges JR, Haag JD, Kosloski-Tarpenning KA, Mara KC, McCoy RG. Gaps in Glucagon Fills among Commercially Insured Patients Receiving a Glucagon Prescription. Diabetes Res Clin Pract. 2023; 200:110720. [PMC10278149]
- Galindo RJ, Uppal TS, McCoy RG, Umpierrez GE, Ali MK. Use and continuity of weight-modifying medications among adults with diabetes and overweight/obesity: US population study. Obesity. 2023;31(12):2924-2935. [PMC10840906]
- Benning TJ, Heien HC, Herges JR, Creo AL, Al Nofal A, McCoy RG. Glucagon fill rates and cost among children and adolescents with type 1 diabetes in the United States, 2011-2021. Diabetes Res Clin Pract. 2023;206:111026. [PMC10872944]
- Everhart AO, Brito JP, Clarke BL, Herrin J, Karaca-Mandic P, Kennel KA, Parimi N, Rosen CJ, Takagi M, McCoy RG. Trends in Osteoporosis Drug Therapy Receipt Among Commercial and Medicare Advantage Enrollees in the United States, 2011-2022. J Clin Endocrinol Metab. 2025 Jan 15
- McCoy RG, Vandergrift JL, Gray B. Patient and physician factors driving the gaps in use of drugs with cardiovascular and kidney benefits by Medicare beneficiaries with type 2 diabetes treated by endocrinologists, nephrologists, and cardiologists: Population-based cohort study. Diabetes Res Clin Pract. 2025 Mar;221:112039
- McCoy RG, Peterson SM, Borkenhagen LS, Takahashi PY, Thorsteinsdottir B, Chandra A, Naessens JM. Which Readmissions May Be Preventable? Lessons Learned From a Posthospitalization Care Transitions Program for High-risk Elders. Med Care. 2018; 56 (8):693-700 [PMC6050026]
- Chen CY, Naessens JM, Takahashi PY, McCoy RG, Borah BJ, Borkenhagen LS, Kimeu AK, Rojas RL, Johnson MG, Visscher SL, Cha SS, Thorsteinsdottir B, Hanson GJ. Improving Value of Care for Older Adults With Advanced Medical Illness and Functional Decline: Cost Analyses of a Home-Based Palliative Care Program. J Pain Symptom Manage. 2018; 56(6):928-935
- Chandra A, Rahman PA, Sneve A, McCoy RG, Thorsteinsdottir B, Chaudhry R, Storlie CB, Murphree DH Jr, Hanson GJ, Takahashi PY. Risk of 30-Day Hospital Readmission Among Patients Discharged to Skilled Nursing Facilities: Development and Validation of a Risk-Prediction Model. J Am Med Dir Assoc. 2019; 20 (4):444-450.e2 [PMC6476539]
- Thorsteinsdottir B, Peterson SM, Naessens JM, Mccoy RG, Hanson GJ, Hickson LJ, Chen CY, Rahman PA, Shah ND, Borkenhagen L, Chandra A, Havyer R, Leppin A, Takahashi PY. Care Transitions Program for High-Risk Frail Older Adults is Most Beneficial for Patients with Cognitive Impairment. J Hosp Med. 2019; 14(6):329-335 [PMC6546541]
- Chandra A, Takahashi PY, McCoy RG, Hanson GJ, Chaudhry R, Storlie CB, Roellinger DL, Rahman PA, Naessens JM. Use of a Computerized Algorithm to Evaluate the Proportion and Causes of Potentially Preventable Readmissions Among Patients Discharged to Skilled Nursing Facilities. J Am Med Dir Assoc. 2021; 22 (5):1060-1066
- Chandra A, Takahashi PY, McCoy RG, Thorsteinsdottir B, Hanson GJ, Chaudhry R, Rahman PA, Storlie CB, Murphree DH Jr. Risk Prediction Model for 6-Month Mortality for Patients Discharged to Skilled Nursing Facilities. J Am Med Dir Assoc. 2022; 23 (8):1403-1408 [PMC9378493]
- Jang S, McCoy RG, Chen J. Prescription Drug Costs Among People With Alzheimer Disease and Related Dementias. JAMA Netw Open. 2024;7(9):e2433026. [PMC11393716]
- Jang S, Qin X, Park S, McCoy RG, Chen J. Healthcare expenditures among older immigrants in the US with Alzheimer’s disease and related dementias: Population-based study between 2007 and 2020. J Gerontol B Psychol Sci Soc Sci. 2024:79(12):gbae166. [PMC11632365]
- Rodriguez-Gutierrez R, Herrin J, Lipska KJ, Montori VM, Shah ND, McCoy RG. Racial and Ethnic Differences in 30-Day Hospital Readmissions Among US Adults With Diabetes. JAMA Netw Open. 2019;2(10):e1913249. [PMC6804020]
- Kurani SS, McCoy RG, Lampman MA, Doubeni CA, Finney Rutten LJ, Inselman JW, Giblon RE, Bunkers KS, Stroebel RJ, Rushlow D, Chawla SS, Shah ND. Association of Neighborhood Measures of Social Determinants of Health With Breast, Cervical, and Colorectal Cancer Screening Rates in the US Midwest. JAMA Netw Open. 2020;3(3):e200618. [PMC7063513]
- Kurani SS, McCoy RG, Inselman JW, Jeffery MM, Chawla S, Finney Rutten LJ, Giblon RE, Shah ND. Place, Poverty and Prescriptions: A Cross-Sectional Study Using Area Deprivation Index to Assess Opioid Use and Drug-Poisoning Mortality in the USA From 2012 to 2017. BMJ Open. 2020;10(5):e035376. [PMC7239546]
- Kurani SS, Lampman MA, Funni SA, Giblon RE, Inselman JW, Shah ND, Allen S, Rushlow D, McCoy RG. Association Between Area-Level Socioeconomic Deprivation and Diabetes Care Quality in US Primary Care Practices. JAMA Netw Open. 2021;4(12):e2138438. [PMC8717098]
- Kurani SS, Heien HC, Sangaralingham LR, Inselman JW, Shah ND, Golden SH, McCoy RG. Association of Area-Level Socioeconomic Deprivation With Hypoglycemic and Hyperglycemic Crises in US Adults With Diabetes. JAMA Netw Open. 2022;5(1):e2143597. [PMC8767428]
- Jiang DH, Herrin J, Van Houten HK, McCoy RG. Evaluation of High-Deductible Health Plans and Acute Glycemic Complications Among Adults With Diabetes. JAMA Netw Open. 2023;6(1):e2250602. [PMC9860518]
- McCoy RG, Swarna KS, Jiang DH, Van Houten HK, Chen J, Davis EM, Herrin J. Enrollment in High Deductible Health Plans and Incident Diabetes Complications. JAMA Network Open. 2024; 7(3):e243394. [PMC10960199]
- Steiger K, Herrin J, Swarna KS, Davis EM, McCoy RG. Disparities in Acute and Chronic Complications of Diabetes Along the U.S. Rural-Urban Continuum. Diabetes Care. 2024;47(5):818-825 [PMC11043221]
- Stickler ZR, Carlson PN, Myers L, Schultz JR, Swenson T, Darling C, Liedl C, McCoy RG. Community Paramedic Mobile COVID-19 Unit Serving People Experiencing Homelessness. Ann Fam Med. 2021;19(6):562. [PMC8575525]
- Ridgeway JL, Wissler Gerdes EO, Zhu X, Finnie DM, Wiepert LM, Glasgow AE, Torres AE, Smith OA, Juntunen MB, Liedl CP, McCoy RG. A Community Paramedic Clinic at a Day Center for Adults Experiencing Homelessness. NEJM Catalyst Innovations in Care Delivery. 2023: 4(4).
- Severson S, Fink A, McCoy R, Liedl C, Bieber P, Juntunen M, Chen H, Lin G. Community Paramedic Home Care Program for Acute Decompensated Heart Failure: A Pilot Study. Circ Cardiovasc Qual 2023;16(9):e009142
- McCoy RG, Nori VS, Smith SA, Hane CA. Development and validation of health impact: an incident diabetes prediction model based on administrative data. Health Serv Res. 2016; 51(5):1896-1918. [PMC5034198]
- McCoy RG, Ngufor C, Van Houten HK, Caffo B, Shah ND. Trajectories of Glycemic Change in a National Cohort of Adults With Previously Controlled Type 2 Diabetes. Med Care. 2017; 55 (11):956-964. [PMC5640500]
- Ngufor C, Houten HV, Caffo BS, Shah ND, McCoy RG. Mixed Effect Machine Learning: a framework for predicting longitudinal change in hemoglobin A1c. J Biomed Inform. 2019;89:56-67. [PMC6495570]
- Yao X, Rushlow DR, Inselman JW, McCoy RG, Thacher TD, Behnken EM, Bernard ME, Rosas SL, Akfaly A, Misra A, Molling PE, Krien JS, Foss RM, Barry BA, Siontis KC, Kapa S, Pellikka PA, Lopez-Jimenez F, Attia ZI, Shah ND, Friedman PA, Noseworthy PA. Artificial intelligence-enabled electrocardiograms for identification of patients with low ejection fraction: a pragmatic, randomized clinical trial. Nat Med. 2021;27(5):815-819
- McCoy RG, Faust L, Heien HC, Patel S, Caffo B, Ngufor C. Longitudinal Trajectories of Glycemic Control among U.S. Adults with Newly Diagnosed Diabetes. Diabetes Res Clin Pract. 2023;205:110989. [PMC10842883]
- McCoy RG, Swarna KS, Deng Y, Herrin J, Ross JS, Kent D, Borah B, Crown W, Montori, VM, Umpierrez G, Galindo RJ, Brito Campana JP, Mickelson M, Polley EC. Derivation of an Annualized Claims-Based Major Adverse Cardiovascular Event Estimator (ACME) in Type 2 Diabetes. JACC: Advances. 2024; 3(4):100852
Chixiang Chen, PhD
Throughout my career, I have been devoted to advancing statistical and data science methods in large-scale data (e.g., Medicare Claims, UK Biobank), encompassing diverse areas such as causal inference, machine learning, federated learning, survival data analysis, missing data analysis, and omics data analysis. My extensive collaborations span various fields, including aging, gerontology, angiology, bioinformatics, biochemistry, and neuroscience, among others. My dedication to research has resulted in over 20 first-author/corresponding peer-reviewed publications, over 70 co-authored publications in total. I am also the recipient of the 2024 Early Career Award from Association for Clinical and Translational Statisticians, honorable mention award of 2024 ICSA China conference, and High Value Early Career Faculty Award for the 2023-2024 term from the National Pepper Older Americans Independence Centers (OAIC). I am the PI in multiple NIH funded projects, including R01 focusing on post-fracture recovery for older adults living with ADRD.
Our group within the Center for Population Health focuses on developing novel analytical methods in health data science. The developed methods aim to better:
- Depict multi-level heterogeneity for treatment effects;
- Identify high-risk subcohorts experiencing poor health outcomes;
- Detect time-varying treatment/exposure effects;
- Examine the comparative effectiveness and safety of different interventions and therapeutic approaches in real-world patient populations;
- Predict and evaluate biological (as opposed to chronological) age.
Our application focuses on (but not limited to) the following populations
- Older adults living with high frailty, e.g., AD/ADRD;
- Patients with multimorbidity;
- Patients with cardiovascular diseases, diabetes, and obesity.
The developed methods / methods under development include (but not limited to)
- Integrating multivariate secondary/surrogate outcomes;
- Casual inference and machine learning;
- Integrating summary information from external data;
- Target trail emulation.
Our group also offers collaboration services and consulting, including (but not limited to)
- (Time varying) propensity score matching/weighting for treatment/exposure comparison
- Target trial emulation
- Real-world evidence/data integration
- Time-to-event analysis with time-varying covariates
- Prediction of multivariate outcomes using machine learning
- Epidemiological design
Recent work
- Deng, D., Zhang, L., Feng, H., Chinchilli, V., , C.*, Wang, M. (2025) Improving Estimation Efficiency for Survival Data Analysis by Integrating a Coarsened Time-to-Event Outcome from an External Study. Biometrics. Accepted.
- Chen, C., Murphy, T. E., Speiser, J. L., Bandeen-Roche, K., Allore, H., Travison, T. G., … & Shardell, M. (2025) Gerontologic Biostatistics and Data Science: Aging Research in the Era of Big Data. The Journals of Gerontology: Series A. 80(1), glae269.
- Chen, C., Chen, S., Long, Q., Das, S., & Wang, M. (2024). Multiple-model-based robust estimation of causal treatment effect on a binary outcome with integrated information from secondary outcomes. The American Statistician, 78(2), 150-160.
- Shardell, M., Chen, C., McCoy, RG. (2024). Doubly robust causal modeling: An application of the technique to evaluate device implantation. JAMA Internal Med, In press.
- McCormick, N., Yokose, C., Lu, N., Wexler, D. J., Aviña-Zubieta, J. A., De Vera, M. A., …,Chen, C.,…, & Choi, H. K. (2024). Comparative effectiveness of sodium-glucose cotransporter-2 inhibitors for recurrent nephrolithiasis among patients with pre-existing nephrolithiasis or gout: target trial emulation studies. BMJ, 387.
Danielle Powell, AuD PhD
Dr. Danielle Powell is a dual-trained Audiologist and Epidemiologist. She received her AuD from the University of North Carolina-Chapel Hill and practiced in the greater Washington D.C. area for several years before pursuing a PhD in Epidemiology from the Johns Hopkins Bloomberg School of Public Health with a focus on epidemiology of aging and a post-doctoral fellowship in health services and outcomes research in the Department of Health Policy and Management at Johns Hopkins as a Health Services and Outcomes Research T32 fellow. Her research is at the intersection of hearing and hearing care, gerontology, epidemiology and public health, dementia, caregiving, health services and health systems-level care. She has a strong interest in the translation of research to clinical care.
Ongoing Research
- Epidemiology of hearing loss and chronic conditions in older adults, including dementia, depression and diabetes
- The relationship between hearing loss and the caregiving experience
- Characterizing how older adults with hearing loss engage with the health system and healthcare providers
- Strategizing innovative ways to facilitate improved integration of hearing as a health concern through electronic medical record or digital health technology tools
Recent Work
- Powell DS, Brenowitz WD, Yaffe K, Armstrong NM, Reed NS, Lin FR, et al. Examining the Combined Estimated Effects of Hearing Loss and Depressive Symptoms on Risk of Cognitive Decline and Incident Dementia. Journal of Gerontology: Series B. 2022 May. 77(5): 839-849. Doi: 1093/geronb/gbab194
- Powell, D.S., Oh, E.S., Lin, F.R. et al. Hearing Impairment and Cognition in an Aging World. JARO. 2021 Jul. 22(4): 387-403.org/10.1007/s10162-021-00799-y.
- Powell DS, Wu MJ, Nothelle S, Smith JM, Gleason K, et al. The Medicare Annual Wellness Visit: An Opportunity to Improve Health System Identification of Hearing Loss? JAGS. 2024. Doi:10.1111/jgs.19111.
- Powell DS, Reed NS, Wolff JL. Care for Hearing Loss in Best Principles of Dementia Care: The Time is Right for Inclusion. JAMDA. 2022; 23(12): e13-e14.
- Powell DS, Reed NS. Sensory loss rehabilitation among those with dementia: a low risk opportunity to move the needle on quality of life. Lancet Healthy Longevity. 5: 2024. org/10.1016/j.lanhl.2024.100640.
Alexandria Ratzki-Leewing, PhD, MSc
Dr. Alexandria Ratzki-Leewing is a tenure-track Assistant Professor in the Division of Gerontology, Department of Epidemiology and Public Health, at the University of Maryland School of Medicine. She holds affiliate appointments with the University of Maryland Institute for Health Computing, the Clinical and Translational Research Informatics Center, and the Center for Research on Aging. She is also an Adjunct Research Professor in the Department of Epidemiology and Biostatistics, Schulich School of Medicine & Dentistry, Western University (London, Ontario, Canada).
Her research centers on capturing and analyzing person-reported data to quantify the real-world burden of diabetes and medication-related side effects across sociodemographically and clinically heterogeneous adult populations. Her methodological expertise includes diabetes (pharmaco)epidemiology, real-world survey design and implementation, and person-reported outcome measures. She also brings deep experience in scientific communication and cross-sector knowledge translation. She has led large-scale, interdisciplinary projects across more than 10 countries, with findings published in leading medical journals and cited in major clinical practice guidelines, including the American Diabetes Association (ADA) Standards of Care.
Dr. Ratzki-Leewing is Deputy Chair of the International Hypoglycaemia Study Group, a senior author of the forthcoming ADA textbook on hypoglycemia, and the 2023 recipient of the International Diabetes Center’s Rising Star award. She has delivered over 100 research presentations globally, developed numerous continuing medical education programs, and regularly contributes to international conference planning and scientific leadership in diabetes.
She earned her PhD in Epidemiology and Biostatistics from Western University (London, Ontario, Canada) in 2023, and her MSc in Health Research Methodology (with a sub-specialization in Health Services Research) from McMaster University (Hamilton, Ontario, Canada).
Selected studies:
- iSTOP Hypo: The upcoming iSTOP Hypo (Identifying Subgroups and Trends to Optimize the Prevention of Hypoglycemia) study targets critical knowledge gaps in the prevention and long-term impact of Level 3 (severe) hypoglycemia. Using advanced analytic techniques and real-world data from iNPHORM, OptumLabs®, and the University of Maryland Medical System, it aims to identify high-risk subgroups, track their clinical trajectories, and estimate the potential benefits of reducing hypoglycemic events. The study also examines how advanced diabetes technologies may modify risk and improve both clinical and patient-reported outcomes. Findings will inform targeted, equity-focused strategies to optimize care and reduce the burden of severe hypoglycemia in diverse diabetes populations.
- iNPHORM: The iNPHORM study (Investigating Novel Predictions of Hypoglycemia Occurrence Using Real-world Models) is a pioneering US-wide, year-long prospective survey designed to assess and predict hypoglycemia risk among adults with type 1 or insulin and/or secretagogue-treated type 2 diabetes. Conducted from 2020 to 2021, it leveraged monthly web-based questionnaires to collect self-reported data on hypoglycemia events, treatment regimens, and various sociodemographic and clinical factors. The study’s main objectives included determining the incidence of Level 3 and non-severe hypoglycemia and developing related prediction models.
- InHypo-DM: The InHypo-DM (Investigating Hypoglycemia in Diabetes Mellitus) study is Canada’s largest real-world investigation into hypoglycemia among adults with diabetes. Conducted in collaboration with colleagues at Western University (Canada), it drew on person-reported data from the InHypo-DM Person with Diabetes Mellitus Questionnaire (InHypo-DMPQ) to examine the incidence and impact of both non-severe and severe hypoglycemic events in individuals with type 1 or type 2 diabetes treated with insulin and/or secretagogues.
Zafar Zafari, MSc, PhD
Dr. Zafari is a quantitative outcomes researcher and health economist with interests in a wide range of applied and theoretical topics in health economics, outcomes research, and health policy including developing simulation models for cost-effectiveness or comparative effectiveness of health policies or technologies, methods of causal inference and causal machine learning, Bayesian methods of synthesizing and reconciling evidence, statistical methods of longitudinal analyses, prospective, or retrospective studies including multi-level (hierarchical) modeling, age-period-cohort analysis, non- or semi-parametric modeling to address burning epidemiological and health policy questions.
Our Postdoctoral Fellows
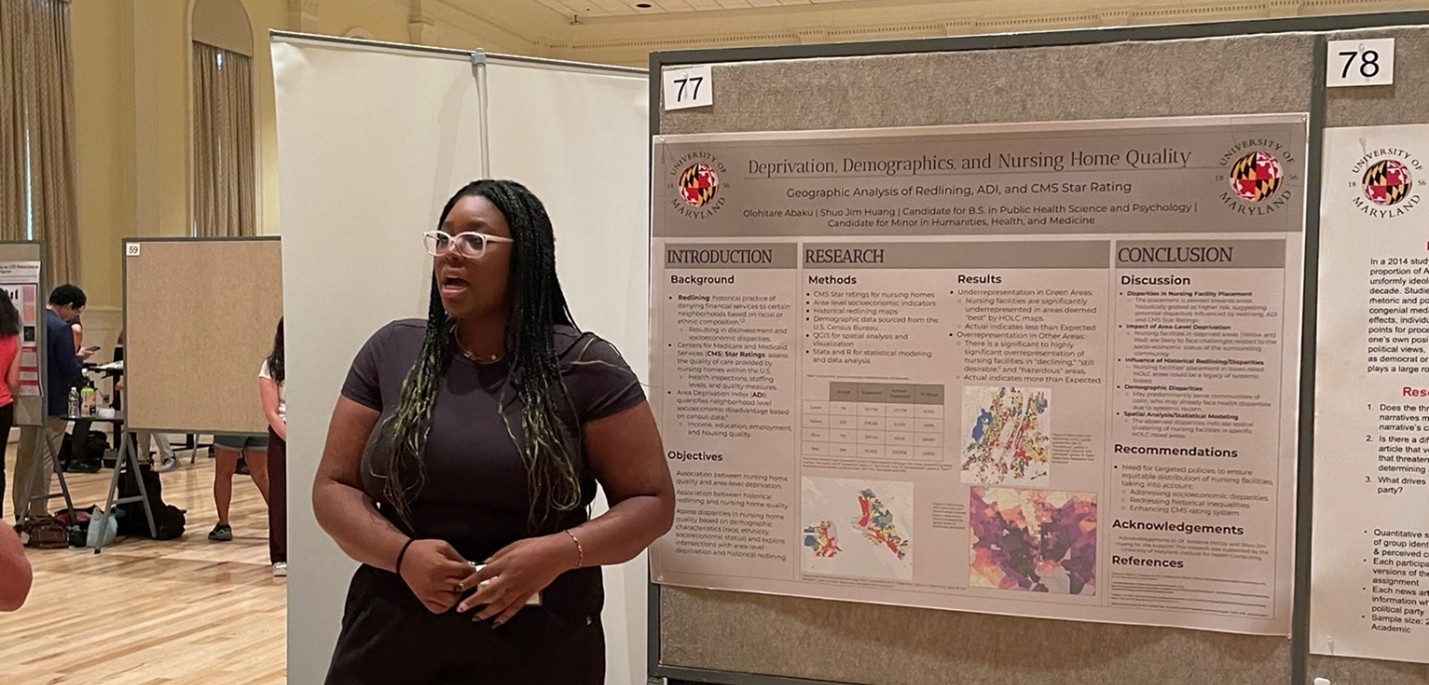
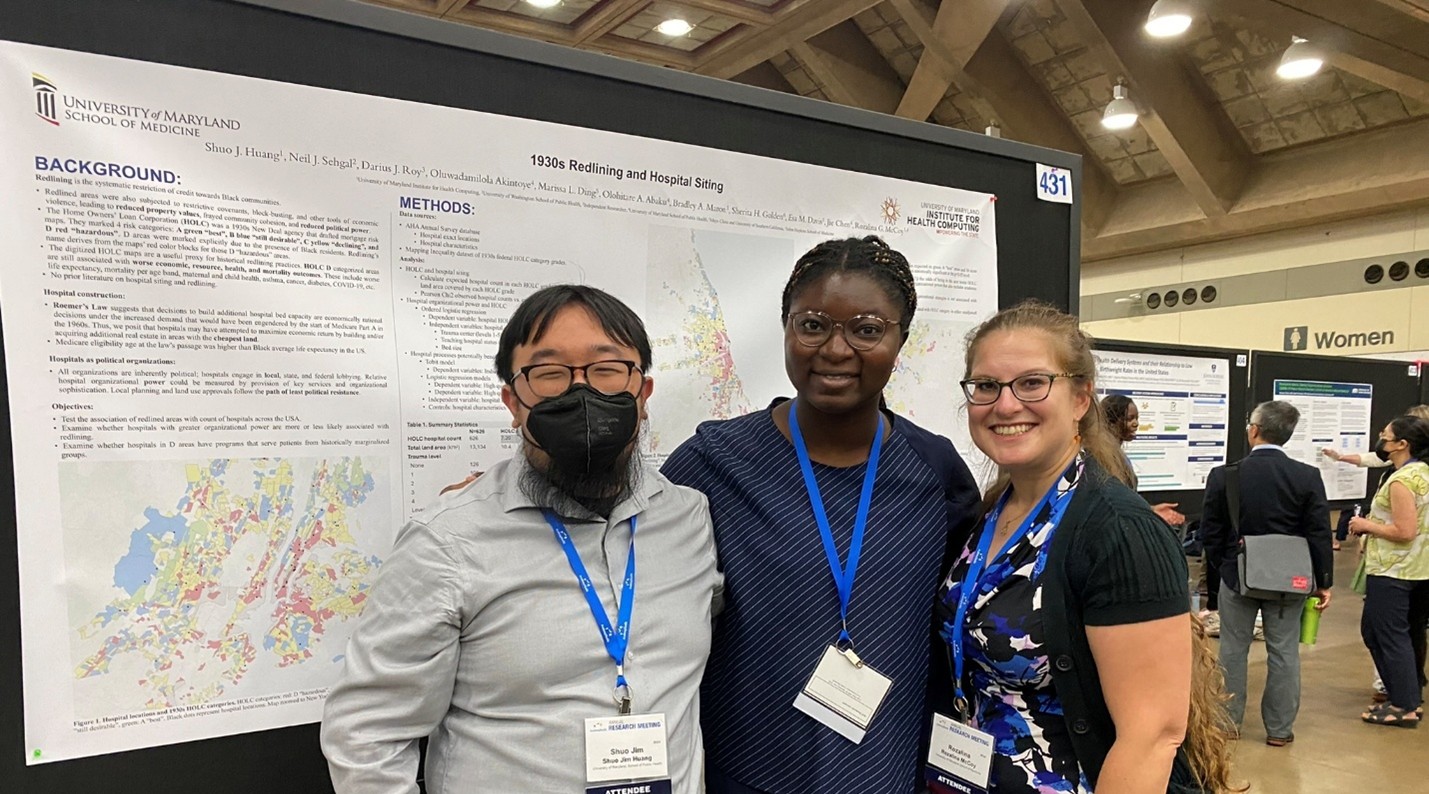
Shuo (Jim) Huang, MPH PhD (mentor: Dr. Rozalina McCoy): structural and social determinants of health
Kaitlynn Robinson-Ector, MPH PhD (mentor: Dr. Rozalina McCoy): implementation and impacts of comprehensive primary care on the quality of care and health outcomes
Renhao Wang, PhD MPH MPA CPH (mentor: Dr. Rozalina McCoy): impact of the Inflation Reduction Act on diabetes management, costs, and outcomes.
Tong Wen, PhD (mentor: Dr. Chixiang Chen): environmental effects on healthy aging
Our Staff
Rui Zhang, MS
Our Students
Doctoral Students
Parth Rastogi (mentor: Dr. Chixiang Chen): fairness-based causal inference
Daxuan Deng (mentor: Dr. Chixiang Chen): s information integration from secondary outcomes
Yilin Zhang (mentor: Dr. Chixiang Chen): causal trajectory analysis
Jeffery Zhao (mentor: Dr. Chixiang Chen): federated learning with causal inference
Haoyu Ren (mentor: Dr. Chixiang Chen): causal machine learning with a continuous exposure
Medical Students
Sinan Aktay (UMSOM)
Elisha Barrientos (UMSOM)
Urja Kalathiya (UMSOM)
Umailla Naeem (UMSOM)
Tahreem Riaz (UMSOM)
Aditi Singh (UMSOM)
Stacey Sklepinski (UMSOM)
Undergraduates
Abby Abaku (UMD)
Matthew Bandos (UMD)
Sean Chun (UMD)
Avishi Gupta (UMD)
Alicia Hawkins (UMD)
Grace Huang (UMD)
Davi Jacobs (UMD)
Haley Ko (UMD)
Jay Sampat (UMD)
Kathleen Tokar (UMD)